PTSD Awareness Month
June Story Spotlight
For our June Story Spotlight, we spoke with retired U.S. Army Veteran, Matt Pech – founder of Operational Athlete Inc. and Ruck for Veterans. Matt is a former Green Beret from Southern California who served for 15 years with 12 of those years on a Special Forces Operational Detachment Alpha (ODA). During this time, Matt experienced nine deployments, four of which were combat rotations to Iraq and Afghanistan. As we continue to raise awareness of PTSD and Veteran suicide, Matt shares his experiences with post-traumatic stress, his own personal growth, resiliency and motivation. Matt is passionate about Veteran-centric non-profits, wellness, fitness, PTS awareness and Veteran suicide prevention.
Depicting The Invisible | A Closer Look
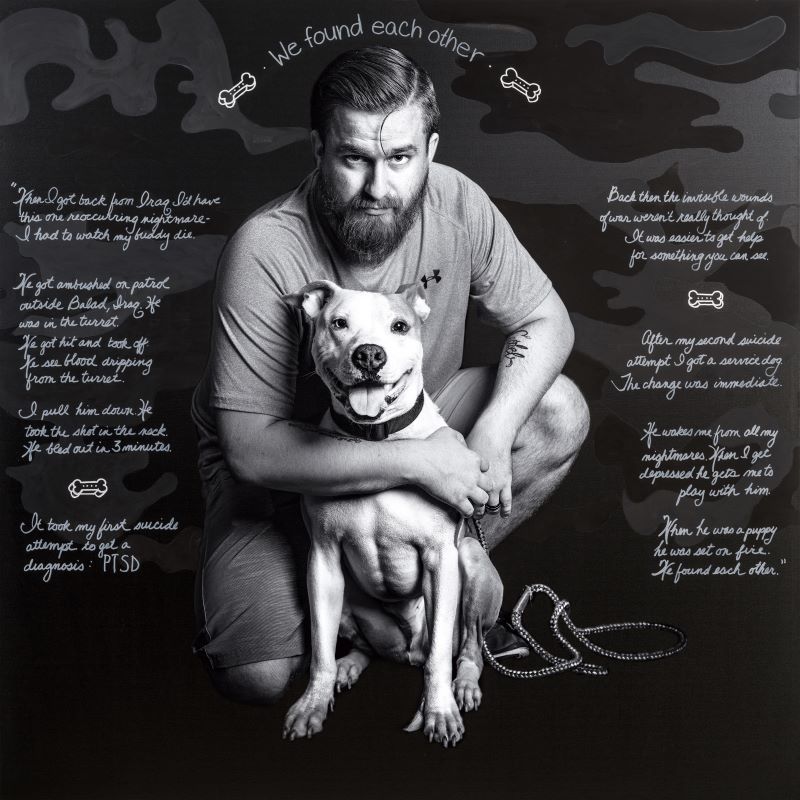
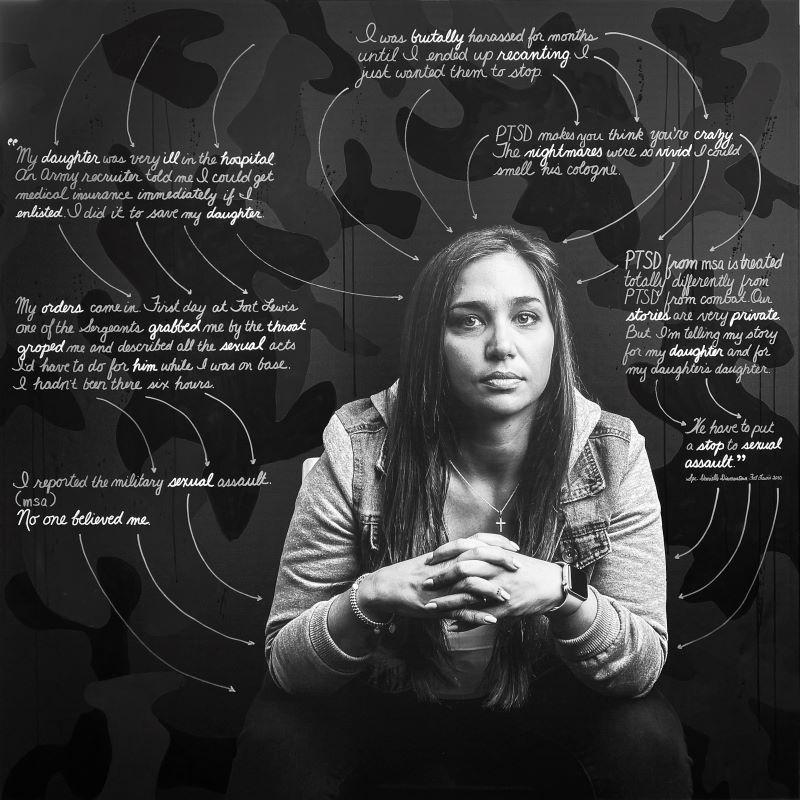
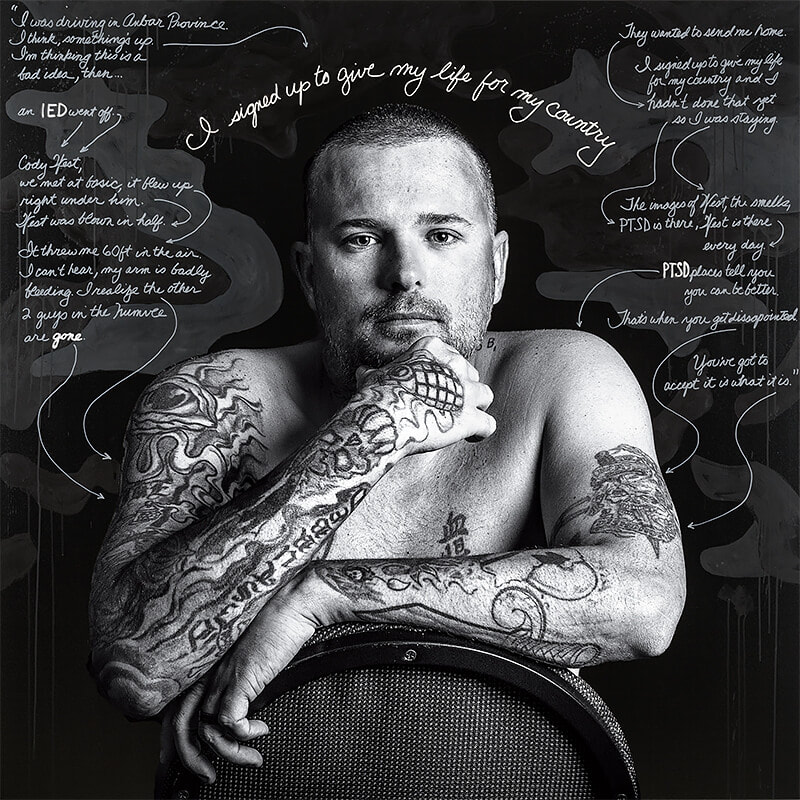
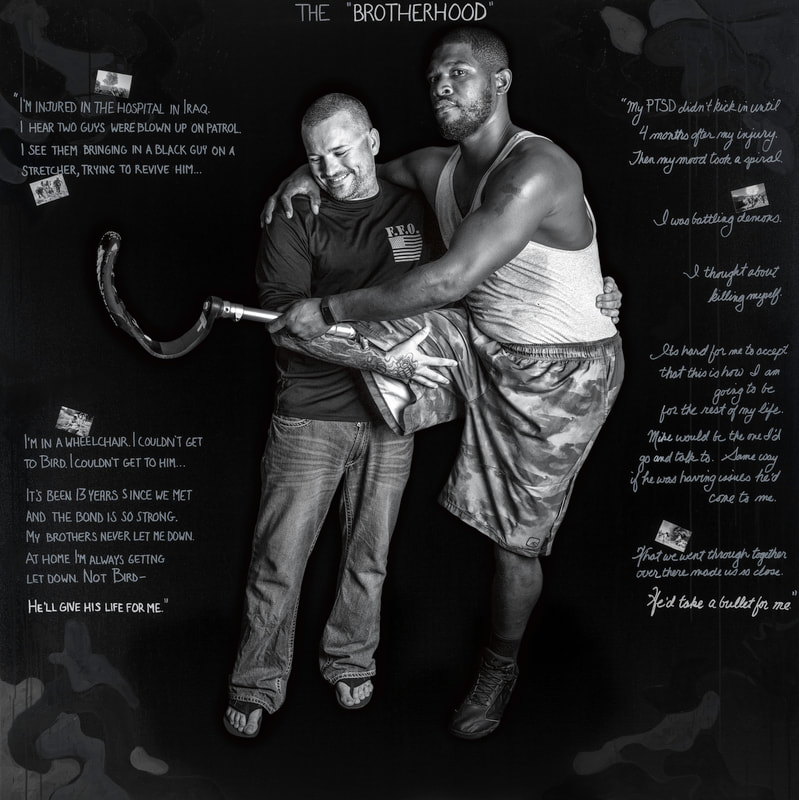
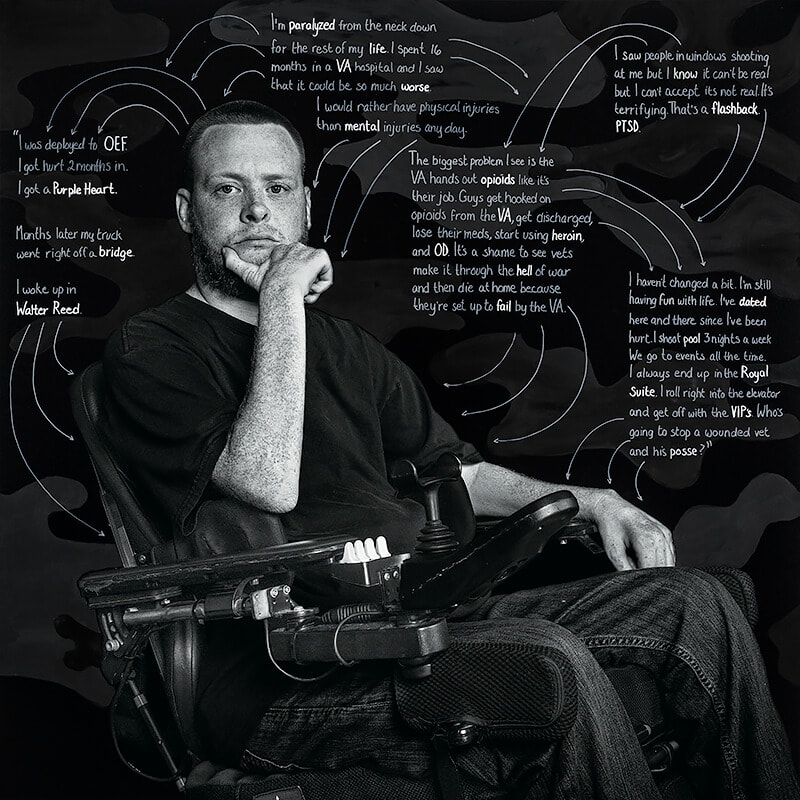
In recognition of PTSD Awareness Month, our Exhibitions Team shares a closer look at Depicting The Invisible: A Portrait Series of Veterans Suffering from PTSD. Each week, hear from a featured Veteran in their own words about their experiences with Post Traumatic Stress. Depicting The Invisible shines a light on these Veterans as they share their personal narratives in order to help other Veterans tell their own stories and seek treatment when they need it most.
Connect with Josh’s Story
This week, we hear from Josh – a U.S. Army Veteran who was diagnosed with PTSD and Traumatic Brain Injury (TBI) when an improvised explosive device (IED) detonated under his vehicle on a routine mission in Iraq.
Connect with Danielle’s Story
Danielle never deployed overseas. Her PTSD stems from military sexual assault (MSA). Danielle shares that, “PTSD from MSA is treated totally different from PTSD from combat. Our stories are very private. But I’m telling my story for my daughter and my daughter’s daughter.”
Connect with Ken’s Story
Ken is a U.S. Army Veteran and Purple Heart recipient. His unit was tasked with locating IEDs and landmines and then detonating them. On June 18, 2004, Ken was in a Humvee (HMMWV) when his arm was hit and severed in an attack. Each year since then, Ken celebrates his Alive Day – the day he didn’t die.
Connect with Rusty’s Story
We close out this four-part series with words from Rusty, who enlisted in the U.S. Army and was awarded the Purple Heart for wounds he sustained in Afghanistan in June, 2010. Months later in January of 2011, the truck he was traveling in went off a bridge and fell fifty feet down a ravine. Rusty spent 16 months at a VA hospital and is paralyzed from the neck down. Rusty says that he, “…would rather have physical injuries than mental injuries any day.”
Inspiring Stories of Service

Josh Sandor
Former U.S. Army Staff Sgt. Joshua Sandor was born and raised in the town of West Milford in northern New Jersey. After graduating from high school in 2001, Josh joined the Army at age 17. In August, he attended basic training at Fort Knox, Kentucky, to become a cavalry scout. “I remember my recruiter trying to tell me about all of these great jobs and career paths I could take, and I had to stop him mid-sentence,” Sandor recalls. “I wanted to be a scout. I already knew that was what I wanted to do.”
On September 11, 2001, Josh found himself on the qualifying range for rifle marksmanship when the terrorist attacks on the World Trade Center began to unfold. In his words, “Our chaplain came out to our range after a post-wide cease-fire was directed for all range operations. We all felt something was wrong and later, as our chaplain spoke, we knew our time on the range was not just to qualify, but to prepare for war…
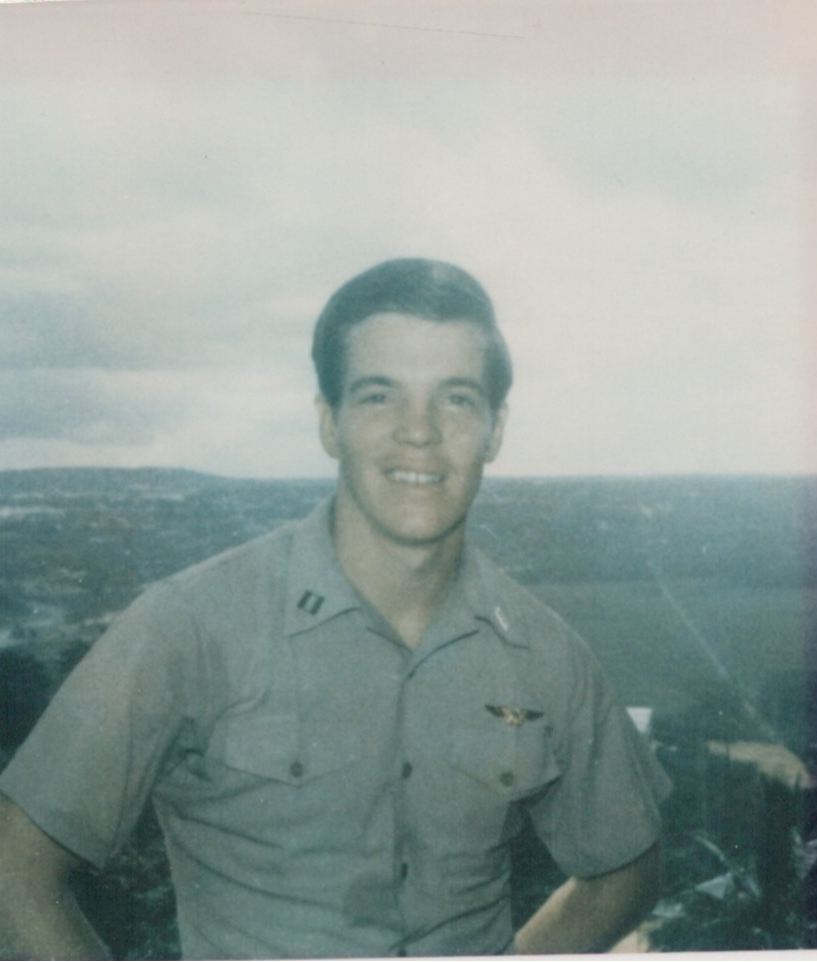
Joseph Whitaker
I led what many would consider an idyllic childhood, the second child of a growing family playing in the apple orchards of Pennsylvania with my siblings and friends. I was struggling inside, however, to win the approval of my disciplinarian father, which did not come easily. I preferred theater to sports, loved being gregarious and making others laugh, and while I had meaningful relationships with women, I knew I was gay from an early age.
I was not always comfortable in my own shoes, but I always knew them to be my shoes and owned my circumstances. Although it took decades for me to fully understand this, accepting my circumstances allowed me to persevere through my many challenges. I felt bullied, unwanted and a failure to my father, yet I continued to fight those feelings, as hard as that would be, and for as long as it would take.
In part, to demonstrate my resolve to myself and others, I enlisted in the U.S. Navy and trained in Pensacola, Florida. I graduated first in my class in 1967 with my father standing beside me. While my older brother avoided the draft and railed against the war, I felt a call to serve in a leadership capacity…
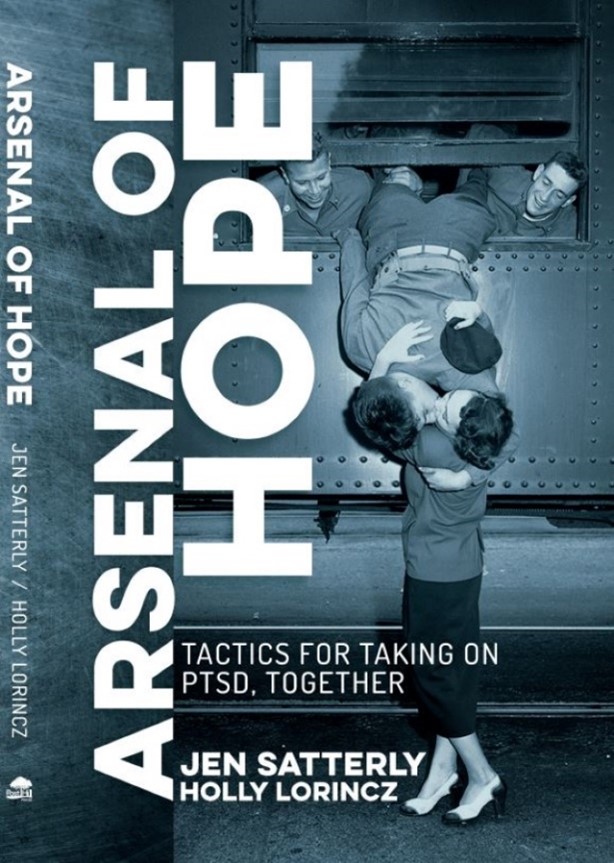
PTSD Awareness Month | What We’re Reading
As we continue to amplify awareness of post-traumatic stress disorder (PTSD), this month’s reading recommendation is dedicated to the military spouses and families who experience secondary traumatic stress, (emotional stress that results from indirect exposure to PTSD and traumatic events). “Arsenal of Hope: Tactics for Taking on PTSD, Together,” co-authored by Jen Satterly and Holly Lorincz serves as a guide to empowering families to work together to heal their individual and collective traumas. In this book, Jen shares countless hours of research and real-life examples from her own personal experiences with PTSD to help Veterans, first responders, civilians, and their families work together to overcome trauma.
Jen Satterly is a compassionate advocate for Veterans and their families. As CEO and co-founder of the All Secure Foundation, she works alongside her husband, Command Sgt. Maj. Tom Satterly, U.S. Army (Retired) who served for 25 years, 20 of those in 1st Special Forces Operational Detachment-Delta (Delta Force). Jen served as director of film and photography embedding with Special Operations units during realistic training missions for three years before founding All Secure to help warriors and their families heal from war trauma on the homefront. This month, Meagan McGowan, our digital exhibitions manager, had the opportunity to connect with Jen about her experiences writing “Arsenal of Hope” following the release of Tom’s book, “All Secure,” published in 2019…
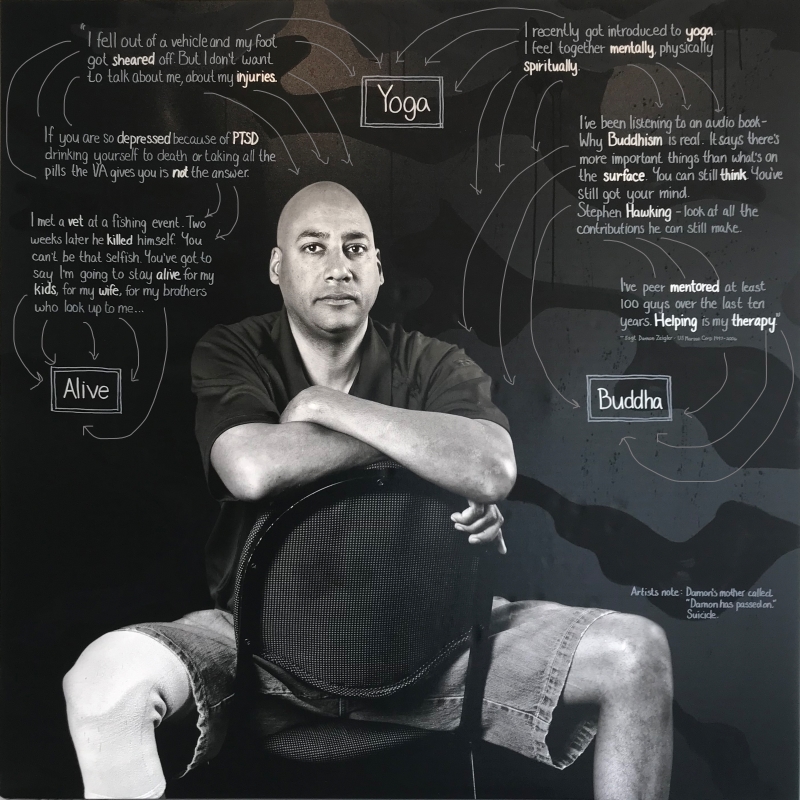
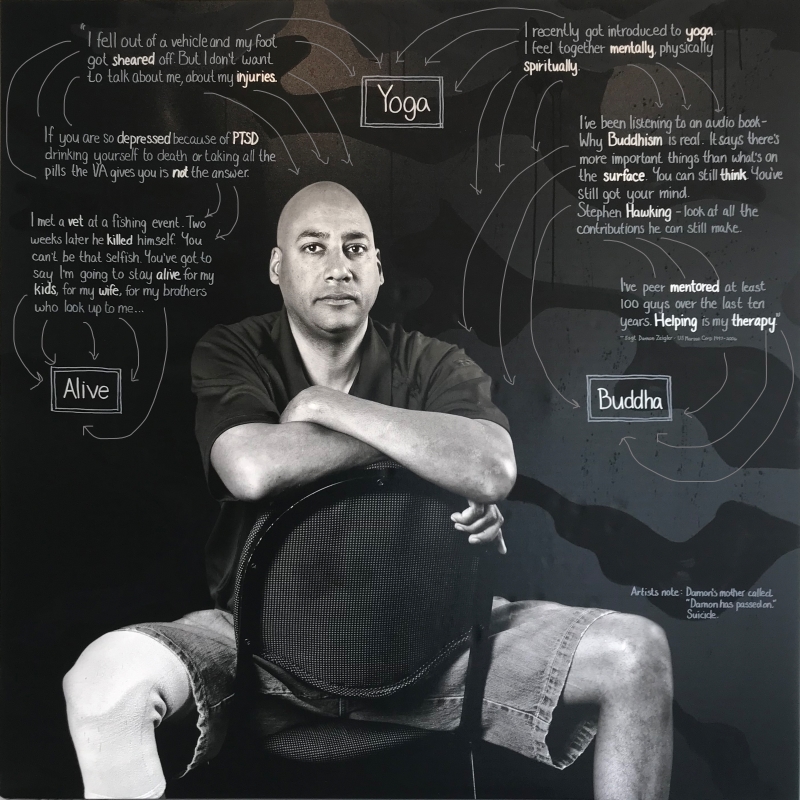
Depicting The Invisible: A Portrait Series of Veterans Suffering From PTSD
April 3, 2021 – February 1, 2022
Depicting The Invisible: A Portrait Series of Veterans Suffering From PTSD by artist Susan J. Barron opens to the public on April 3. Barron was inspired to create the portrait series after hearing that 22 Veterans commit suicide every day in our country.
“My intention is to bring awareness to the issues of PTSD and to depict our Veterans as the incredible heroes they are,” said Barron. “… My mission is to provide a platform for Veterans to share their stories, and to create a vehicle for help and change.”
Her series of 14 hauntingly beautiful six-foot by six-foot, mixed media works on canvas are created through a combination of photographic imagery, paint and text including each Veteran’s story. Each Veteran in these portraits makes unflinching eye contact with the viewer to showcase them as powerful and vulnerable as they share the truth of their realities in their own words.
Depicting The Invisible is shown at the museum as part of our ongoing mission to share the Veteran experience through their own stories. We are partnering with Susan J. Barron to create a dialogue and community around the stigmas associated with war’s invisible scars to show these brave individuals they are not alone, end their isolation and represent them as the heroes they are.
About the Artist
Susan J. Barron is an exceptionally diverse, multi-award-winning artist whose work has been collected and commissioned across the nation. Whether working with oil on canvas, photographic processes, or incorporating sculpture and collage elements, her work bravely and beautifully explores the intersection of the viewer’s preconception and reality.
She has had solo exhibitions throughout the United States, including the Hunter Museum of Art, TN, HG Contemporary Gallery, NY, Caelum Gallery, NY, the Kevin Butler Gallery in Massachusetts, the First Frontier Collage Society in Texas, and the Lark Creek Gallery in California. A graduate of Boston University, she studied art at the Art Institute of San Francisco and Yale School for the Arts. She is currently traveling the country with her latest body of work, Depicting The Invisible.

Thank you to our Exhibition Sponsors
Virtual Tour
MEMBERS, redeem your special access to the Depicting The Invisible Virtual Tour using this link. To join as a member, click here. With questions about MEMBER ACCESS to this tour, email members@nationalvmm.org.
Saturday, April 3 – Friday, December 31
Depicting The Invisible: A Portrait Series of Veterans Suffering From PTSD
During this 21-minute tour, you will hear the personal narratives of Veterans living with PTSD. We provide a platform for Veterans to share their stories, and to create a vehicle for help and change. Our virtual tour is proudly presented by CAS – A division of the American Chemical Society. Virtual tickets are available through December 31, 2021, and cost $7 for 72 hours of tour access. The tour is free for museum members.
Virtual Events
In recognition of PTSD Awareness Month, we invite you to join the conversation on Post-Traumatic Stress Disorder (PTSD), suicide prevention, treatment and intervention. Our June 5 Rally Point will feature Magnus Johnson, a U.S. Army Veteran and former Green Beret, and Chief Strategy Officer of Mission 22, whose mission is to support the Veteran community with three main programs: Veteran treatment programs, memorials and community social impact. In addition, leaders in innovative treatments for suicide and trauma for military personnel, Veterans and first responders at The Ohio State University Veterans Craig Bryan, PsyD, ABPP and AnnaBelle Bryan, MS will join the conversation. Learn more about how we can all make a difference in the lives of those who served our nation.
As a part of PTSD Awareness Month, Veteran and Gold Star Spouse Jennifer Ballou hosts a hybrid yoga session at the National Veterans Memorial and Museum. This program includes a brief introduction and a 45-minute Restorative Flow yoga class, followed by closing remarks on how yoga and mindfulness tie into physical wellness and mental health.
SATURDAY, APRIL 3 – FRIDAY, DECEMBER 31
Depicting The Invisible: A Portrait Series of Veterans Suffering From PTSD
During this 21-minute tour, you will hear the personal narratives of Veterans living with PTSD. We provide a platform for Veterans to share their stories, and to create a vehicle for help and change. Our virtual tour is proudly presented by CAS – A division of the American Chemical Society. Virtual tickets are available through December 31, 2021, and cost $7 for 72 hours of tour access. The tour is free for museum members.
What is PTSD?
“Post-Traumatic Stress Disorder (PTSD) is a mental health problem that some people develop after experiencing or witnessing a life-threatening event, like combat, a natural disaster, a car accident or sexual assault.” – U.S. Department of Veterans Affairs
“Post-Traumatic Stress Disorder (PTSD) is a mental health condition that’s triggered by a terrifying event – either experiencing it or witnessing it.” – Mayo Clinic
Causes and Symptoms
Causes
You can develop Post-Traumatic Stress Disorder when you go through, see or learn about an event involving actual or threatened death, serious injury or sexual violation. Anyone can develop PTSD at any age. Doctors aren’t sure why some people get PTSD while others don’t. A number of factors can increase the chance that someone will have PTSD, many of which are not under that person’s control. For example, having a very intense or long-lasting traumatic event or getting injured during the event can make it more likely that a person will develop PTSD. As with most mental health problems, PTSD is probably caused by a complex of:
- Stressful experiences, including the amount and severity of trauma you’ve gone through in your life.
- Inherited mental health risk, such as a family history of anxiety and depression.
- Inherited features of your personality – often called your temperament.
- The way your brain regulates the chemicals and hormones your body releases in response to stress.
Kinds of Traumatic Events
The most common events leading to the development of PTSD include:
- Combat exposure
- Childhood physical abuse
- Sexual violence
- Physical assault
- Being threatened with a weapon
- An accident
Many other traumatic events can also lead to PTSD, such as fire, natural disaster, mugging, robbery, plane crash, torture, kidnapping, life-threatening medical diagnosis, terrorist attack and other extreme or life-threatening events.
Symptoms
Symptoms of PTSD may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks. There are four major types of symptoms: re-experiencing, avoidance, hyperarousal, and negative changes in beliefs and feelings.
Re-Experiencing, Reliving, or Intrusive Memories
Memories of traumatic event can come back at any time. You may feel the same fear and horror you did when the event took place. For example:
- You may have nightmares.
- You may feel like you are going through the event again. This is called a flashback.
- You may see, hear, or smell something that causes you to relive the event. This is called a trigger. News reports, seeing an accident, or hearing a car backfire are examples of triggers.
- You may have recurrent, unwanted distressing memories of the traumatic event.
Avoidance
You may try to avoid situations or people that trigger memories of the traumatic event. You may even avoid talking or thinking about the event. For example:
- You may avoid crowds, because they feel dangerous.
- You may avoid driving if you were in a car accident or if your military convoy was bombed.
- If you were in an earthquake, you may avoid watching movies about earthquakes.
- You may keep very busy or avoid seeking help because it keeps you from having to think or talk about the event.
Hyperarousal or Being on Guard
You may be jittery, or always alert and on the lookout for danger. You might suddenly become angry or irritable. This is known as hyperarousal. For example:
- You may have a hard time sleeping.
- You may have trouble concentrating.
- You may be startled by a loud noise or surprise.
- You might want to have your back to a wall in a restaurant or waiting room.
- Irritability, angry outbursts or aggressive behavior.
- Overwhelming guilt or shame.
- Self-destructive behavior, such as drinking too much or driving too fast.
Negative Changes in Beliefs and Feelings
The way you think about yourself and others changes because of the trauma. This symptom has many aspects, including the following:
- You may not have positive or loving feelings towards yourself or other people and may stay away from relationships.
- You may forget about parts of the traumatic event or not be able to talk about them.
- You may think the world is completely dangerous, and no one can be trusted.
- Feeling detached from family and friends.
- Lack of interest in activities you once enjoyed.
- Difficulty experiencing positive emotions or feeling emotionally numb.
PTSD Symptoms in Children
Children may have symptoms described above or other symptoms depending on how old they are. As children get older, their symptoms are more like those of adults. Here are some examples of PTSD symptoms in children:
- Children under 6 may get upset if their parents are not close by, have trouble sleeping, or act out the trauma through play.
- Children 7 to 11 may also act out the trauma through play, drawings, or stories. Some have nightmares or become more irritable or aggressive. They may also want to avoid school or have trouble with schoolwork or friends.
- Children age 12 to 18 have symptoms more similar to adults: depression, anxiety, withdrawal, or reckless behavior like substance abuse or running away.
Treatment
Post-Traumatic Stress Disorder treatment can help you regain a sense of control over your life. The primary treatment is psychotherapy, but can also include medication. Combining these treatments can help improve your symptoms by:
- Teaching you skills to address your symptoms.
- Helping you think better about yourself, others, and the world.
- Learning ways to cope if any symptoms arise again.
- Help you make sense of the trauma.
- Help you reconnect with people you care about.
- Treating other problems often related to traumatic experiences, such as depression, anxiety, or misuse of alcohol or drugs.
You don’t have to try to handle the burden of PTSD on your own. For additional ways to find help with PTSD, please visit the “Get Help” tab at the top of the page.
How Can I Help Someone With PTSD?
When someone you care about has PTSD, it affects you too. You are probably spending time and energy to help your loved one cope. Even if your partner, family member, or friend with PTSD is getting treatment and getting better, you may still feel drained, worried, or even frustrated. You need support at the same time you are giving support.
Remember that you can’t change someone. However, you can:
- Learn about PTSD. This can help you understand what your loved one is going through.
- Recognize that avoidance and withdrawal are part of the disorder. If your loved one resists your help, allow space and let your loved one know that you’re available when he or she is ready to accept your help.
- Offer to attend medical appointments. If your loved one is willing, attending appointments can help you understand and assist with treatment.
- Be willing to listen. Let your loved one know you’re willing to listen, but you understand if he or she doesn’t want to talk. Try not to force your loved one to talk about the trauma until he or she is ready.
- Encourage participation. Plan opportunities for activities with family and friends. Celebrate good events.
- Make your own health a priority. Take care of yourself by eating healthy, being physically active and getting enough rest. Take time alone or with friends, doing activities that help you recharge.
- Seek help if you need it. If you have difficulty coping, talk with your doctor. He or she may refer you to a therapist who can help you work through your stress.
- Stay safe. Plan a safe place for yourself and your children if your loved one becomes violent or abusive.
Get Help
Get Help in a Crisis
- Call 9-1-1
- Go to the nearest Emergency Room
- Contact the National Suicide Prevention Lifeline: 1-800-273-8255. En Espanol: 1-888-628-9454
- Contact the Veterans Crisis Line:
- 1-800-273-8255, press 1
- Send a text to 838255
- Chat online through the Confidential Veterans Chat
Find a Therapist
Things to Consider:
- If you are a Veteran, see Help for Veterans.
- Make sure the provider has experience treating people who have been through a trauma.
- Try to find a provider who focuses on evidence-based medications for PTSD or effective talk therapy for PTSD.
- Find out what type(s) of insurance the provider accepts and what you will have to pay (out-of-pocket costs) for care.
- You may find more than one therapist. Learn about Types of Therapists.
First Steps:
- Contact your family doctor to ask for a recommendation. Or, ask friends and family if they can recommend a therapist.
- If you have health insurance, call to find out which mental health providers your insurance company will cover. Your insurance company may require that you choose a provider from a list they maintain.
Finding a Provider Using the Internet
These resources can help you locate a therapist, counselor or mental health provider who is right for you. Note: These resources can be used by anyone, and if you are a Veteran, see the “Help for Veterans” section below.
- Sidran Institute Help Desk will help you find therapists who specialize in trauma treatment. Call the Help Desk at 410-825-8888.
- Anxiety and Depression Association of America offers a therapist search by location and mental health disorder. Call 240-485-1011.
- EMDR International Association has a locator that lists EMDR providers.
- ISTSS Clinician Directory is a service provided by the International Society for Traumatic Stress Studies (ISTSS) that lets you consider many factors in searching for a clinician, counselor or mental health professional.
- American Psychological Association has a Psychologist Locator that allows you to search by location, specialty, insurance accepted and gender of the provider.
- Psychology Today offers a therapist directory by location. You can also find treatment centers.
- Substance Abuse and Mental Health Services Administration (SAMHSA) offers a Behavioral Health Services Locator by location and type of facility (inpatient, outpatient, residential). Call for assistance 24-hours a day at 1-800-662-HELP (4357).
Finding a Provider by Phone
In addition to the numbers listed above, you can also find a therapist, counselor or mental health provider in the following ways:
- Some mental health services are listed in the phone book. In the Government pages, look in the “County Government Offices” section, and find the “Health Services (Dept. of)” or “Department of Health Services”. “Mental Health” or “Behavioral Health” will be listed.
- In the yellow pages, mental health providers are listed under “counseling”. “psychologists”, “social workers”, “psychotherapists”, “social and human services”, “mental health” or “behavioral health”.
- You can also call the psychology department of a local college or university.
Help for Veterans
- All VA Medical Centers and many VA clinics provide PTSD care.
- Some VA centers have specialty programs for PTSD. Use the VA PTSD Program Locator to find a VA PTSD program.
- Vet Centers provide readjustment counseling to Veterans and their families after war. Find a Vet Center near you.
- VA Medical Centers and Vet Centers are also listed in the phone book. In the Government pages, look under “United States Government Offices”. Then look for “Veterans Affairs, Dept of”. In that section, look under “Medical Care” and “Vet Centers – Counseling and Guidance”.
- If you are a Veteran looking for a community care provider, learn more about VA’s MISSION Act.
- Find more information on Help for Veterans.
Some of the Resources Available on PTSD
Mission 22
The Suicide and Trauma Reduction Initiative for Veterans (STRIVE)
medicine.osu.edu/departments/psychiatry-and-behavioral-health/strive
National Suicide Prevention Helpline
suicidepreventionlifeline.org | 800.273.8255
U.S. Department of Veterans Affairs Readjustment Counseling
vetcenter.va.gov | 800.273.8255 (Press 1)
National Sexual Assault Hotline
rainn.org | 800.656.4673
Make the Connection
Ohio Alliance to End Sexual Violence
oaesv.org | 888.886.8388
Alcohol, Drug and Mental Health Board of Franklin County
adamhfranklin.org | 614.224.1057
Veteran Companion Animal Services
Mental Health America Franklin County
mhaohio.org | 614.884.7227
LOSS Community Services
losscs.org | 614.530.8064