PTSD Awareness
We all have a role to play in listening, connecting and reaching out to those who may be struggling with challenges. By talking about mental health and suicide, it not only helps reduce stigma and increase awareness, but it also has the potential to save a life.
Post-Traumatic Growth: Finding Purpose through Fitness [Rally Point]
This June, we’re raising awareness about post-traumatic stress and helping to reduce the stigma to…
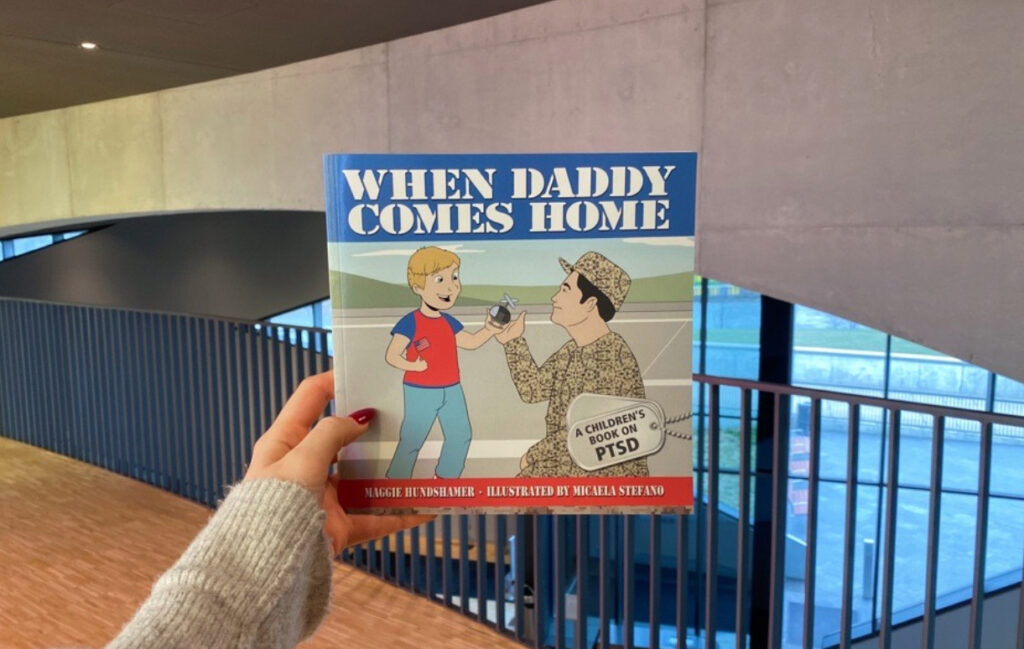
NVMM Reads: “When Daddy Comes Home: A Children’s Book on PTSD”
“When Daddy Comes Home” by U.S. Marine Corps Veteran, Maggie Hundshamer, uses plain language to…
We can stop Veteran suicide. It starts with understanding.
A Special Message from our President and CEO September is Suicide Prevention Awareness Month, a…
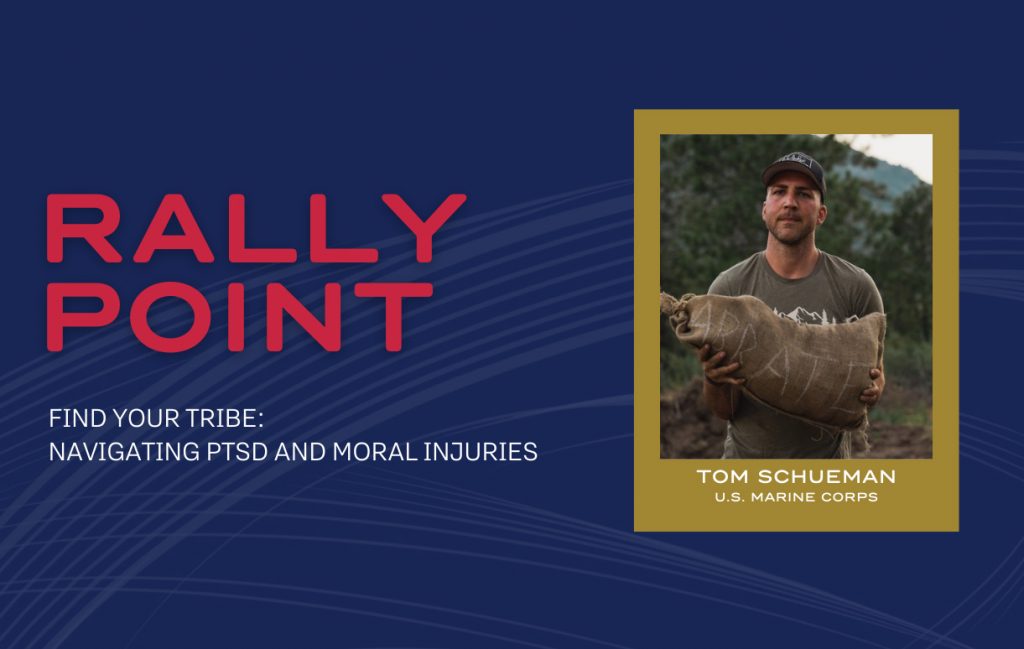
Find Your Tribe: Navigating PTSD and Moral Injuries [Rally Point]
The month of June is dedicated to bringing awareness to Post-traumatic Stress and reducing the…
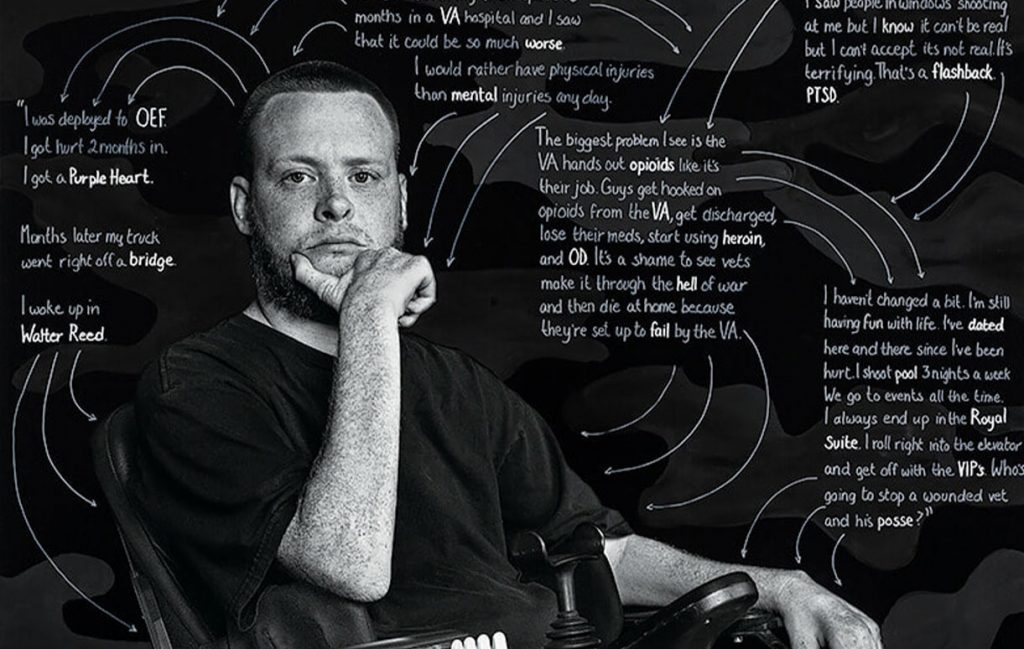
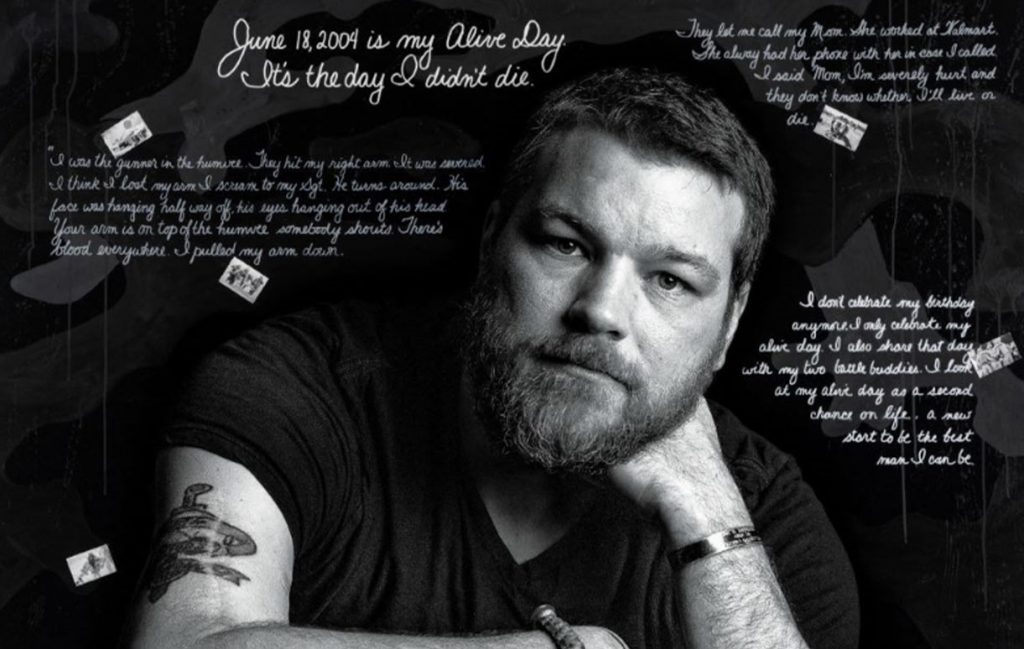
“Depicting the Invisible” Exhibition: Rusty’s Story
In recognition of PTSD Awareness Month, our Exhibitions Team shares a closer look at Depicting The…
Veteran Spotlight: Matt Pech, U.S. Army Veteran
Check out our June Story Spotlight with retired U.S. Army Veteran, Matt Pech – founder…
“Depicting the Invisible” Exhibition: Ken’s Story
In recognition of PTSD Awareness Month, our Exhibitions Team shares a closer look at Depicting The…
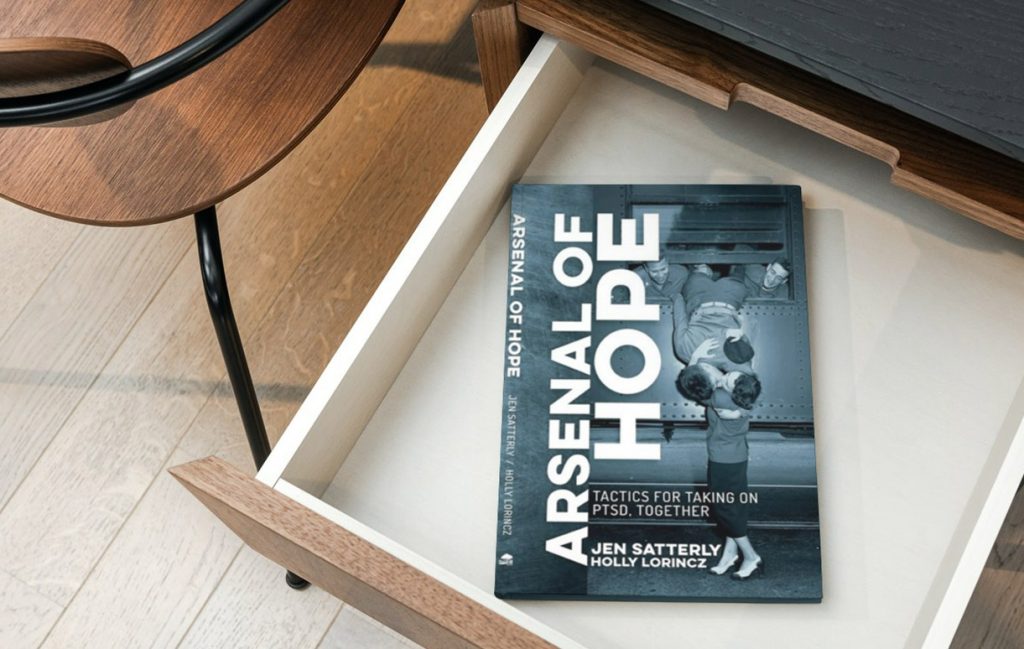
NVMM Reads: “Arsenal of Hope: Tactics for Taking on PTSD, Together”
As we continue to amplify awareness of post-traumatic stress disorder (PTSD), this month’s reading recommendation…
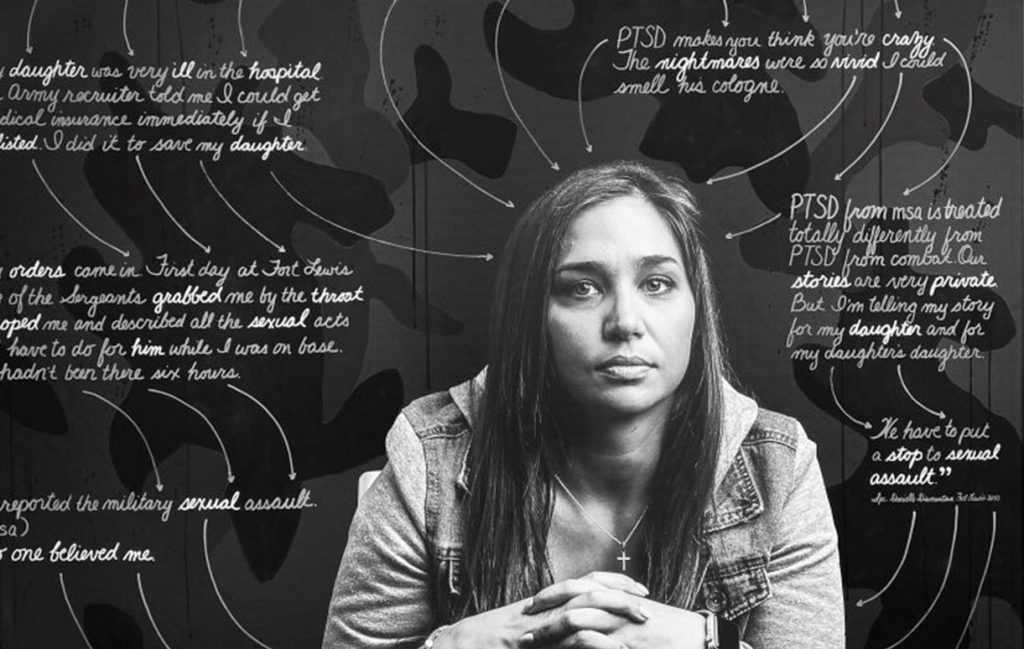
“Depicting the Invisible” Exhibition: Danielle’s Story
In recognition of PTSD Awareness Month, our Exhibitions Team shares a closer look at Depicting…
PTSD Awareness Month | What We’re Reading
As we continue to amplify awareness of post-traumatic stress disorder (PTSD), this month’s reading recommendation…
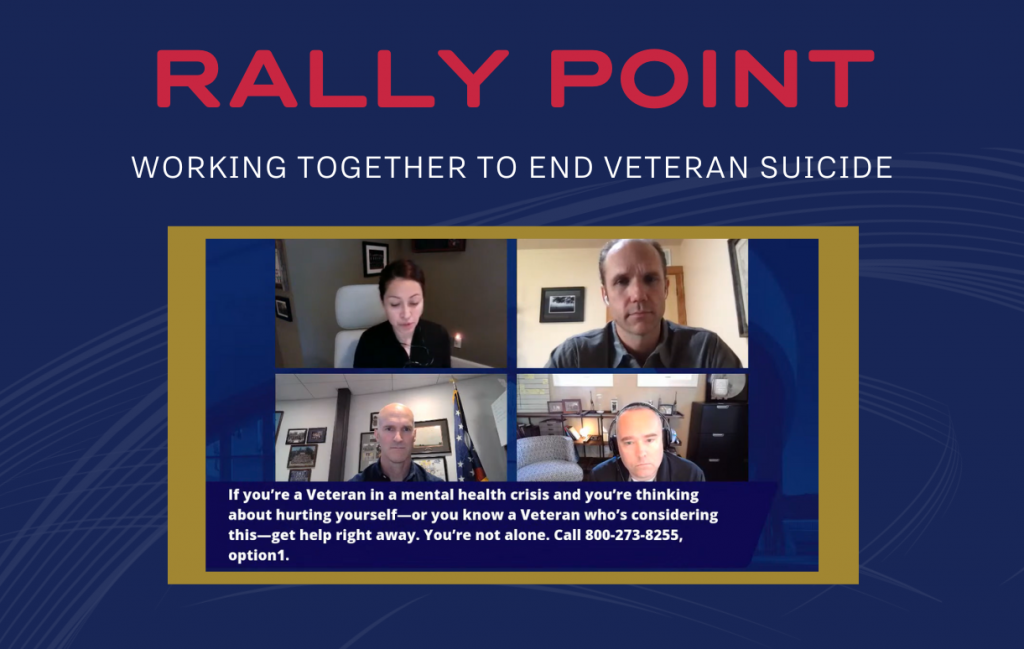
Working Together to End Veteran Suicide [Rally Point]
In recognition of PTSD Awareness Month, we invite you to join the conversation on Posttraumatic…
“Depicting the Invisible” Exhibition: Josh’s Story
Meet Josh – a U.S. Army Veteran who was diagnosed with PTSD and Traumatic Brain…
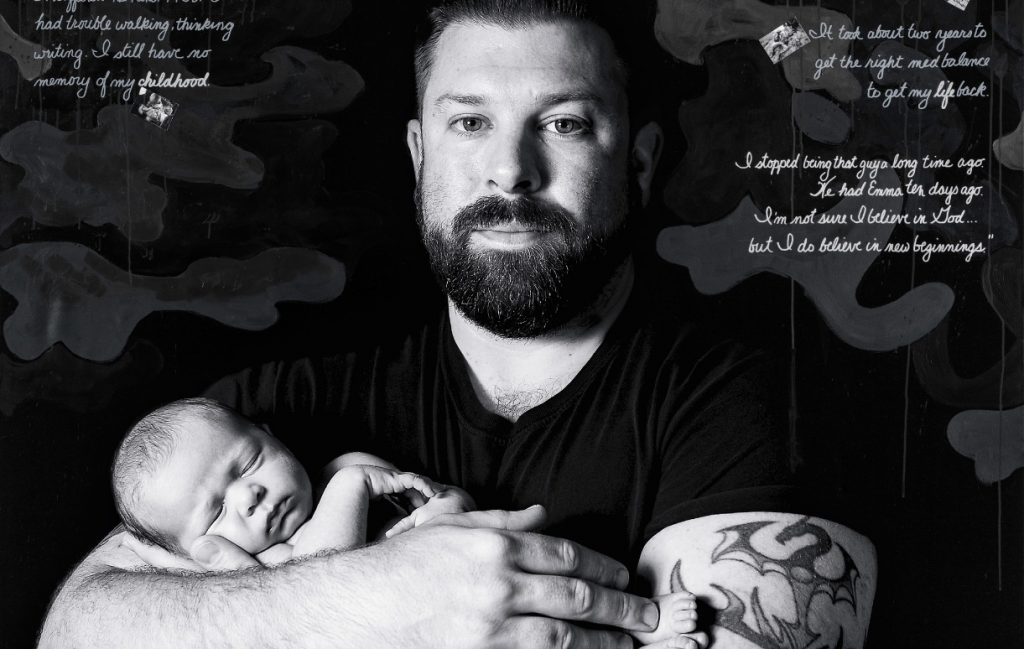
Inspiring Story of Service | PTSD Awareness Month – Josh Sandor
Josh & Emma, 2018 | Mixed media on canvas © Susan J. Barron Former U.S….
No Victim of Circumstances: PTSD Awareness with Joseph Whitaker
by Joseph Whitaker I led what many would consider an idyllic childhood, the second child…
Rally Point – Find Your Tribe: Navigating PTSD and Moral Injuries
The month of June is dedicated to bringing awareness to Post-traumatic Stress and reducing the stigma attached to seeking treatment. Our Rally Point focused on how to “Find Your Tribe: Navigating PTSD and Moral Injuries” with special guest active-duty United States Marine Corps Major Tom Schueman, founder of Patrol Base Abbate.
Rally Point: Working Together to End Veteran Suicide
Our June Rally Point features Magnus Johnson, a U.S. Army Veteran and former Green Beret, and Chief Strategy Officer of Mission 22, whose mission is to support the Veteran community with three main programs: Veteran treatment programs, memorials and community social impact. In addition, leaders in innovative treatments for suicide and trauma for military personnel, Veterans and first responders at The Ohio State University Veterans Craig Bryan, PsyD, ABPP and AnnaBelle Bryan, MS joined the conversation.
The Healing Power of Yoga
As a part of PTSD Awareness Month, Veteran and Gold Star Spouse Jennifer Ballou hosts a hybrid yoga session at the National Veterans Memorial and Museum. This program includes a brief introduction and a 45-minute Restorative Flow yoga class, followed by closing remarks on how yoga and mindfulness tie into physical wellness and mental health.
What is PTSD?
“Post-Traumatic Stress Disorder (PTSD) is a mental health problem that some people develop after experiencing or witnessing a life-threatening event, like combat, a natural disaster, a car accident or sexual assault.” – U.S. Department of Veterans Affairs
“Post-Traumatic Stress Disorder (PTSD) is a mental health condition that’s triggered by a terrifying event – either experiencing it or witnessing it.” – Mayo Clinic
Causes
You can develop Post-Traumatic Stress Disorder when you go through, see or learn about an event involving actual or threatened death, serious injury or sexual violation. Anyone can develop PTSD at any age. Doctors aren’t sure why some people get PTSD while others don’t. A number of factors can increase the chance that someone will have PTSD, many of which are not under that person’s control. For example, having a very intense or long-lasting traumatic event or getting injured during the event can make it more likely that a person will develop PTSD. As with most mental health problems, PTSD is probably caused by a complex of:
The most common events leading to the development of PTSD include:
Many other traumatic events can also lead to PTSD, such as fire, natural disaster, mugging, robbery, plane crash, torture, kidnapping, life-threatening medical diagnosis, terrorist attack and other extreme or life-threatening events.
Symptoms
Symptoms of PTSD may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks. There are four major types of symptoms: re-experiencing, avoidance, hyperarousal, and negative changes in beliefs and feelings.
Re-Experiencing, Reliving, or Intrusive Memories
Memories of traumatic event can come back at any time. You may feel the same fear and horror you did when the event took place. For example:
Avoidance
You may try to avoid situations or people that trigger memories of the traumatic event. You may even avoid talking or thinking about the event. For example:
Hyperarousal or Being on Guard
You may be jittery, or always alert and on the lookout for danger. You might suddenly become angry or irritable. This is known as hyperarousal. For example:
Negative Changes in Beliefs and Feelings
The way you think about yourself and others changes because of the trauma. This symptom has many aspects, including the following:
PTSD Symptoms in Children
Children may have symptoms described above or other symptoms depending on how old they are. As children get older, their symptoms are more like those of adults. Here are some examples of PTSD symptoms in children:
Treatment
Post-Traumatic Stress Disorder treatment can help you regain a sense of control over your life. The primary treatment is psychotherapy, but can also include medication. Combining these treatments can help improve your symptoms by:
You don’t have to try to handle the burden of PTSD on your own. For additional ways to find help with PTSD, please visit the “Get Help” tab at the top of the page.
How can I help someone with PTSD?
When someone you care about has PTSD, it affects you too. You are probably spending time and energy to help your loved one cope. Even if your partner, family member, or friend with PTSD is getting treatment and getting better, you may still feel drained, worried, or even frustrated. You need support at the same time you are giving support.
Remember that you can’t change someone. However, you can:
Resources

The Veterans Crisis Line
A free, confidential, 24-hour hotline for Veterans and their families. Call 1-800-273-8255 or text 383255. Options available for those who are deaf or hard of hearing.